1. 小兒輸液
- 水分
- Infant: 100~120/kg/day (能量需求也差不多是這樣算-->大卡)
- >1 yrs: 100/50/20 rule
- 小朋友血量:85 x kg c.c./ 大人血量: 75 x kg c.c.
- 電解質
- 胞外:鈉氯鈣/ 胞內:鉀磷鎂
- Na, Cl: 2 mEq/kg/day
- Ca, K, P: 1 mEq/kg/day
- Mg: 0.25 mEq/kg/day
- 男>女,先天性肥大,約3~6 wks old
- 成因:缺乏神經叢(alpha plexus)無法窄縮--> proximal part肥大
- 表現:無膽汁嘔吐,右上腹橄欖狀腫塊,代謝性鹼中毒(低血氯、重碳酸高)
- 影像:string sign,超音波則看到pylorus擴大(1.4cm)+muscle增厚(0.4cm)+括約肌長度增加
- 處置:非緊急手術(pyloromyotomy)
- 預後:良好
3. Intussusception
- 好發於6個月到2歲(換副食品)、迴腸套住盲腸
- 風險因子:曾經病毒感染(大人:腫瘤如平滑肌瘤、adenocarcinoma)
- 症狀:陣發性(10~15mins)哭鬧、縮腿蜷曲、currant jelly stool(黏液性血便)、觸摸到腹部香腸狀腫塊
- 影像:contrast enema(兼具治療)--> coil spring sign
- 處置:NPO+ NG decompression+ IV+ antibiotics+ enema(90%成功率/10%復發率),入院觀察24hrs,若失敗則開刀徒手復位
- 好發:男>女(4:1),直腸(10%)、直腸+sigmoid(75%)
- 病因:缺乏神經節(alpha plexus)、相關上游神經增生
- 臨床表現:delayed meconium passage(>48hrs)、腹脹
- 影像:enema-->transitional zone, bizarre contraction, retention of barium> 24~48hrs,不事先灌腸
- 黃金診斷:biopsy(缺乏plexus、acetylesterase↑)
- 處置:避免enterocolitis,需要decompression+ antibiotics,手術處理
- 非緊急手術:two steps (colostomy-> resection-> anastomosis) at 6~12 months(>10kg)
- Swenson
- Duhamel
- Soave
- 胚胎:cloacal membrane在7th week碰觸到perineal body,8th week時開口
- 好發:男>女
- 分類
- 高位:puborectalis以上-->anorectal atresia,容易併膀胱/陰道/尿道fistula
- 低位:puborectalis以下-->anal atresia= membranous type,容易併會陰部fistula(80~90%)
- 影像:up side down X ray--> invertogram
- 處理
- <1cm--> perineal shift in anoplasty
- >1cm--> colostomy, 4~6 months later anoplasty, another 3 months later close colostomy
- 預後:愈高位愈容易incontinence,術後能自由排便70%,然而完全不會滲便只有40%
- 合併症:VACTERL
6. NEC
- 滿月內嬰兒最常見的腹部急症
- 好發於出生後10~30天、terminal ileum、ascending colon
- 風險因子:早產、周產壓力(Infection, Ischemia, Immune)
- 臨床表現:Bell stage
- stage I: n/v
- stage II: abdominal distention and tenderness
- stage III: peritonitis, severe metabolic acidosis, DIC, sepsis

- 影像:pneumatosis intestinalis(經典)、gas in portal vein、fixed dilated bowel、free air(perforated)

- 處置:NPO、NG decompression、fluid support、antibiotic、兩階段手術(if 48~72hr未改善)
- 預後:overall mortality 80%
- 併發症:stricture、short bowel
7. Meconium ileus
- 好發於terminal ileum
- 原因:過於黏稠的meconium
- 風險因子: cystic fibrosis(西方人較多)
- Cl test in sweat >60 mEq/L
- CFTR gene
- 臨床表徵:腹脹、腸阻塞、delayed meconium passage
- 影像:plain film看到GGO(meconium+gas)、enema看到microcolon
- DDx: Hirschsprung disease
- 處置:enema(80%成功率),失敗則開刀注射acetylcysteine+milking腸子
8. Omphalocele vs. Gastroschisis
- 發生率:omphalocele(F>M)> gastroschisis
- 裂口大小:omphalocele(4cm↑)> gastroschisis(3~5cm)
- 合併症:omphalocele(30~70%)> gastroschisis(<10%)
- 死亡率:omphalocele(10~30%)> gastroschisis(5~15%)
- 處置:通常需要呼吸器+PPN、人工膜覆蓋(腹裂)、階段性修補

9. Umbilical hernia
- 自行關閉的條件:2歲以前、1.5cm以下
- 消化道最常見的異常
- 成因:卵黃管的留存,屬於true diverticulum(whole layer)
- 好發:antimesenteric side
- 臨床表現:rule of two (+M>F, 2:1),出血(因為異味胃組織)>堵塞>diverticulitis
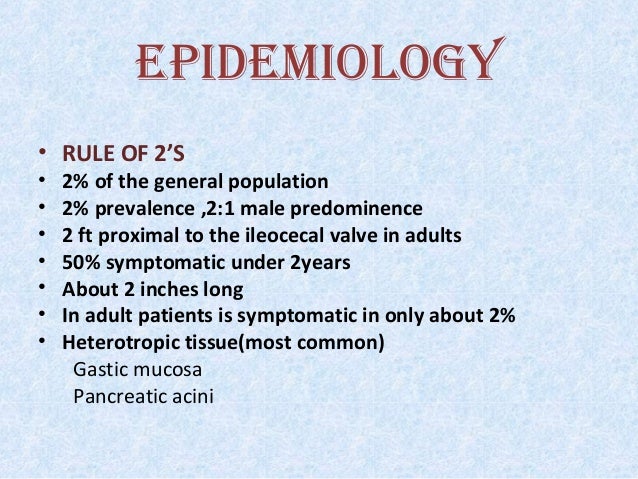
- 處置:有併發症再開刀(segmental resection+ end to end anastomosis),如果摸到的appendix很厚、懷疑有異生組織可一起拿掉
- DDx
- 若通道表皮= umbilico-ileal fistula (有mucus discharge)
- 若近端盲端= umbilical sinus
11. Intestinal atresia
- 好發於十二指腸> 空腸> 迴腸> 結腸
- 分類
- 食道、十二指腸閉鎖(40%併其他異常):true embryologic abnormality
- 其他腸道閉鎖:intrauterine mesenteric vascular (SMA) accident
- 臨床表現:羊水過多、嘔吐、腹脹
- 影像:double bubble sign
- 處置:手術bypass、
- 合併症:30%Down syndrome、20%congenital heart disease,其他腸道閉鎖無合併其他先天異常
- P.S. Down syndrome最常合併的先天異常是congenital heart disease
- 分類(Type C最常見)

- 臨床症狀:羊水過多、第一次餵奶就吐奶、recurrent choking、腹脹
- 影像:plain film- GI gas↑
- 處置:俯臥、頭高、NG decompression、NPO、antibiotics、開刀
- 合併症:40%VACTERL
13. Diaphragm hernia
- 解剖複習
- 最好發於左後外方(Bochdalek hernia),其次在胸骨下方(Morgagni hernia),最後才是esophageal旁的hiatal hernia(大人常見)

- 臨床症狀:肺發育不全、cyanosis、縱膈腔右推、腹部塌陷(scaphoid/empty abdomen)
- 影像:bowel gas in chest
- 處置:NPO、fluid、NG decompression、高濃度呼吸支持(幾乎都需要插管、壓力不能高)
- 預後:mortality 50%(主因為肺部)
14. Choledochal cyst/ biliary atresia
- 好發:女>男(4:1),東方人>西方人
- Types
- I: 85%
- V: intrahepatic duct cystic dilation= Calori disease
- 臨床症狀:黃疸、腹痛(膽管炎、胰臟炎)、腫塊
- 影像:sono+ CT( IHD 增生不會dilation), Tc99m
- DDx: 新生兒肝炎(pathology->giant cell, consider biopsy)
- 處置
- 60天以內,行total excision(Kasai's operation + reconstruction(Y loop)
- transplantation(contraindication:metastatic CA, cirrhosis Child B/C)
- 預後:差
- 葛西式10 year survival rate=53%
- 肝移植10 year survival rate=66.7%
- 是否有膽囊膽道炎是重要因子
15. Wilms' tumor(nephroblastoma)
- 惡性,經血液轉移到肺臟
- 成因:基因突變刪除(Chr. 11= WT-1, WT-2, tumor suppressor gene)
- 好發:peak 3 y/o (1~7 y/o)
- 臨床症狀:腫塊、腹痛
- 影像:sono, CT, pyelography
- 治療:手術、化療,III, IV期+ radiation
- 預後:佳(五到十年存活率: 80~90%)
16. Neuroblastoma(腎上腺髓質、交感神經節後)
- 惡性,經血液轉移到肺臟,屬於APUD(amine precursor uptake and decarboxylation)的一種
- 成因:基因突變(Chr. 2= ameC, oncogene)
- 好發:80%<4y/o, peak 2 y/o,腎上腺髓質、交感神經節(腹部脊椎旁>縱膈腔>頸部)
- 成人最常見腎上腺髓質腫瘤為pheochromocytoma(90%良性),也是APUD tumor
- 臨床症狀:腫塊、catecholamine造成的高血壓
- 檢驗:代謝產物VMA, HMA
- 治療:手術、化療
- 預後:差,survival rate =30%
17. 小兒常見死因
- 創傷
- 癌症:leukemia> brain tumor> neuroblastoma
18. Hepatoblastoma
- 小兒最常見肝臟惡性腫瘤,HCC次之
- 好發:3 y/o 以下 (HCC: 10~15 y/o)
- 檢驗:tumor marker- alpha fetal protein
- 影像:sono, CT
- 治療:手術為主,化療有效(HCC: 相對無效)
- 預後:survival rate =70% (HCC: 25%)
19. Torticollis 斜頸症
- 成因:SCM纖維化
- 大人成因:spasm
- 風險因子:剖腹產,一個月內就會發現
- 臨床表現:患側頸部硬塊,頸彎向患側、頭朝健側
- 治療:復健2~5個月,超過一年未恢復可手術(myotomy劃開)
- 合併症:頸椎、胸椎scoliosis、臉部變形